Accepted Insurances
Patient Forms
Office Policies
Post-op Care & Instructions
We participate in many local and national insurance plans. Please call our office at (909) 748-6065 to verify that we are a participating provider with your insurance plan. Out-of-network visits are also welcome. Special arrangements can be made with most insurance plans.
We currently accept HMO insurances if you are a member of the following medical groups:
Redlands Yucaipa Medical Group
Pinnacle Medical Group
PrimeCare Medical Group
We currently accept the following PPO insurances:
AARP
Access Health Direct
Acordia National
Advance Benefit Resources
Aetna
Aetna US Healthcare
Affilia Healthcare Admin
AFTRA Health Fund
Allied Benefit Systems
Altius Helath Plans
Amerahealth Administrators
Amerbien/IEC Group
American Community
American Insurance Administrators
APWU Health Plan
Assurant Health
Aurora Direct
BeechStreet
Ben Elect
Benefit Administrative Systems
Benefit Advantage
Benefit Plan Administrators
Benesight
Big Lots Associate Benefit Plan
Blue Cross
Blue Shield
BRMS
California Field Ironworkers
CBA
CBCA Administrators
CCN
Cement Masons Claim Office
Champ VA
Christian Care Processing Center
Cigna
Cigna Healthcare
Cinergy Health Inc.
Claims Central
COMM Net Communications
Community Care Network
Comprehensive Care Services
Connecticut General Life Co.
Coresource
Coventry Healthcare
Delta Health Systems
Design Benefits Administrators
EBAM Credit Corp.
EBMS
First Health
FISERV Health
FMH Benefit Services
GEHA
Gilsbar, Inc.
Global Medical Management
Great West
Great West Life and Annuity
Group Resources, Inc.
Guardian
Health Plan, Inc.
Health Plus Insurance Co.
HealthNet
Healthscope Benefits
Hewitt Coleman Associates
Hometown Health
Humana
IAA
IBEW-NECA Health Plan
Independent Health
Insurance Center
Kennan Associates
Labor Trust Fund
Laborers Health and Welfare
Laundry & Dry Cleaning Workers
Lifeguard Insurance
Lifeline Screening of America
Los Angeles Fireman Relief
Lumenos
Major League Baseball
Medical Institute
Medicare
Mid West National Life Insurance Co.
Mo-Kan Sheet Metal Workers
MPI Health
Mutual Assurance Administration
Mutual of Omaha
Nationwide Health Plan
Nationwide Insurance
Nationwide Specialty Health Co.
NBC Health
NGS American
Nippon Life Insurance Co.
NPPN-BAMF
Operating Engineers Health
Oxford Health Plans
Major League Baseball
Medical Institute
Medicare
Mid West National Life Insurance Co.
Mo-Kan Sheet Metal Workers
MPI Health
Mutual Assurance Administration
Mutual of Omaha
Nationwide Health Plan
Nationwide Insurance
Nationwide Specialty Health Co.
NBC Health
NGS American
Nippon Life Insurance Co.
NPPN-BAMF
Operating Engineers Health
Oxford Health Plans
Tall Tree Administrators
TCS
Teamsters Security Fund
The Capella Group
The J.P. Farley Corporation
The Mail Handlers Benefit Plan
The Plan Handlers, Inc.
Time Insurance Company
TPSC
UFCW
UFCW Unions & Food Employers
UniCare
United Agriculture Benefit Trust
United Healthcare
United Medical Resources, Inc.
University of MO Claims
USAA Life Insurance Company
VA MC Fee Services
WASAU Benefits
Washington-Idaho Carpenters
Watkins Associated Industries
WEYCO Inc.
WMI/TPA Care VU
Woodward Healthcare Services
Younglife Benefits
Patient Forms
We are currently welcoming new patients for obstetrical and gynecological care. For your first visit, please arrive about 20 minutes before your appointment time. If you have been under the care of another physician, please have the records sent to us prior to your first appointment. If you are taking medications, please bring the names and dosages with you. You can expedite your visit if you complete the following forms, prior to your appointment. Please call to find out if you need a referral from your Primary Care Physician, before your appointment.
Office Policies
We respect the value of your time and want to spare you long waits. Our specialty does involve emergency procedures, surgical delays, and the least predictable of all, deliveries; consequently, we ask for your understanding. If Dr. Hage is running behind, our staff will try to notify you, or Jeannette Langston, WHNP may be able to see you. You may also call prior to your visit to see if we anticipate any delays. We also request that you arrive promptly for your visit so other patients are not delayed. If you are unable to keep your appointment or are going to be late, please call the office as soon as possible. A cancellation fee will apply if your appointment is not cancelled 24 hours prior.
In the best interest and safety of all of our patients, the following policies will be in effect:
• Patients will ONLY be allowed one (1) guest to accompany them to an appointment.
• Children over the age of 3 months will NOT be allowed in the office- unless it is the patient.
We apologize for any inconvenience this may cause. Guests that are unable to attend the appointment are welcome to wait in the building lobby on either floor or in the cafe located in the pharmacy on the first floor of our building. We will be happy to re-schedule your appointment so that proper child care can be obtained.
If you think you are going to be late for your appointment, please call us ahead of time and we will be happy to reschedule your appointment to another time that is more convenient for you.
Post-Op Care & Instructions
Cesarean Section (C-Section)
WHAT TO EXPECT:
Your back may be sore for a few days from the spinal anesthesia that was used during surgery. If you had general anesthesia, your throat may be sore for a few days from the tube used to put you to sleep. You may also have abdominal and/or shoulder pain from gas that enters your abdomen from having an open surgery. These symptoms are not serious. They will go away within a few days.
INCISIONS:
You have one incision in your belly, usually in the bikini line. If you have tape strips over the incisions, leave them on for 7 days and then remove them. When you shower, let soapy water run over the incision. Afterward, pat it dry. If a strip starts to fall off, it is okay to remove it. It is normal to have bruising around the incisions.
PAIN:
You will get prescriptions for Ibuprofen (Motrin) and a narcotic pain pill (Norco or Tylenol #3.) Take Ibuprofen three times a day, with meals, until you no longer need it. If you need them, take the narcotic pain pills in addition, according to the instructions on the bottle.
DIET:
If you are not hungry, just drink liquids for the first 24 hours. When you are hungry, eat regular food. Drink plenty of water and eat lots of fruits and vegetables to avoid constipation. If eating regular foods gives you gas pains, go back to clear liquids.
ACTIVITY:
You can shower 24 hours after your surgery. Don’t drive for at least 3 weeks after surgery. After that, when you are no longer taking narcotic pain pills, not feeling drowsy, and you can move around quickly without discomfort, you may begin to drive. Do not stay in bed all day. You will heal faster if you get up and move around the house. You may walk up and downstairs- it is not harmful. When you feel ready for a particular activity (such as light housework or exercise) you can try it. You can expect to be able to return to work approximately 4-6 weeks after your surgery.
VAGINAL DISCHARGE and BLEEDING:
It is normal to have some bleeding or discharge from the vagina for up to 4-6 weeks after surgery. You may have a sudden gush of blood about 2 weeks after delivery; this should not last more than 1-2 days; if it does, call the office.
INTERCOURSE:
Do not use tampons or have sexual intercourse until after you have come for a post-op examination. You may resume sexual intercourse after 6 weeks unless instructed otherwise by Dr. Hage.
BOWELS:
It is normal not to have a bowel movement for several days after surgery. To avoid getting constipated, you may drink prune juice or take an over-the-counter product such as milk-of-magnesia or colace.
FOLLOW-UP APPOINTMENT:
If you do not have an appointment when you leave the hospital, call the office the next business day to arrange for an appointment within 2-3 weeks of your surgery.
IF YOU NOTICE ANY of the FOLLOWING:
• Fever > 100.4 on two occasions, 4 hours apart.
• Pus coming out of the incision.
• Vaginal bleeding heavier than a period.
• Pain that is not controlled by the prescribed medicines and/or does not lessen with time.
• Unable to keep down liquids.
• Redness, swelling or bruising around the incision which is worsening day-after-day.
YOU SHOULD:
• Call for a same day appointment
• Go to urgent care.
• Go to the Emergency Room.
To leave a non-urgent message for your physician, call the office.
This information is provided as a resource only and is not intended to be a recommendation or a substitute for consultation with Dr. Hage regarding your health and needs.
Dilation & Curettage (D&C)
WHAT TO EXPECT:
Your throat may be sore for a few days from the breathing tube that was used during surgery. These symptoms are not serious. They will go away within a few days.
PAIN:
You can take Ibuprofen (Motrin) three times a day, with meals, until you no longer need it.
DIET:
If you are not hungry, just drink liquids for the first 24 hours. When you are hungry, eat regular food. Drink plenty of water and eat lots of fruits and vegetables to avoid constipation.
ACTIVITY:
You can shower a few hours after your surgery. Don’t drive for at least 24 hours after surgery. After that, when you are not feeling drowsy, and you can move around quickly without discomfort, you may begin to drive. Do not stay in bed all day unless otherwise instructed by Dr. Hage.
VAGINAL DISCHARGE:
It is normal to have some bleeding or discharge from the vagina for a few days after surgery.
INTERCOURSE:
Do not use tampons or have sexual intercourse until after 6 weeks unless instructed otherwise by Dr. Hage.
BOWELS:
Your bowel function should not be affected after surgery. To avoid getting constipated, you may drink prune juice or take an over-the-counter product such as milk-of-magnesia or colace.
FOLLOW-UP APPOINTMENT:
If you do not have an appointment when you leave the hospital, call the office the next business day to arrange for an appointment within 2-3 weeks of your surgery.
IF YOU NOTICE ANY of the FOLLOWING:
• Fever > 100.4 on two occasions, 4 hours apart.
• Pus coming out of the incision.
• Vaginal bleeding heavier than a period.
• Pain that is not controlled by the prescribed medicines and/or does not lessen with time.
• Unable to keep down liquids.
• Redness, swelling or bruising around the incision which is worsening day-after-day.
YOU SHOULD:
• Call for a same day appointment
• Go to urgent care.
• Go to the Emergency Room.
To leave a non-urgent message for your physician, call the office.
This information is provided as a resource only and is not intended to be a recommendation or a substitute for consultation with Dr. Hage regarding your health and needs.
Hysterectomy – Abdominal
WHAT TO EXPECT:
Your throat may be sore for a few days from the breathing tube that was used during surgery. You may also have abdominal and/or shoulder pain from gas that enters your abdomen from having an open surgery. These symptoms are not serious. They will go away within a few days.
INCISIONS:
You have one incision in your belly, usually in the bikini line. If you have tape strips over the incisions, leave them on for 7 days and then remove them. When you shower, let soapy water run over the incision. Afterward, pat it dry. If a strip starts to fall off, it is okay to remove it. It is normal to have bruising around the incisions.
PAIN:
You will get prescriptions for Ibuprofen (Motrin) and a narcotic pain pill (Norco or Tylenol #3.) Take Ibuprofen three times a day, with meals, until you no longer need it. If you need them, take the narcotic pain pills in addition, according to the instructions on the bottle.
DIET:
If you are not hungry, just drink liquids for the first 24 hours. When you are hungry, eat regular food. Drink plenty of water and eat lots of fruits and vegetables to avoid constipation. If eating regular foods gives you gas pains, go back to clear liquids.
ACTIVITY:
You can shower 24 hours after your surgery. Don’t drive for at least 3 weeks after surgery. After that, when you are no longer taking narcotic pain pills, not feeling drowsy, and you can move around quickly without discomfort, you may begin to drive. Do not stay in bed all day- you will heal faster if you get up and move around the house. You may walk up and downstairs. It is not harmful. When you feel ready for a particular activity (such as light housework or exercise) you can try it. You can expect to be able to return to work approximately 4-6 weeks after your surgery.
VAGINAL DISCHARGE:
It is normal to have some bleeding or discharge from the vagina for a few weeks after surgery.
INTERCOURSE:
DO NOT PUT/INSERT ANYTHING INSIDE THE VAGINA. NO sexual intercourse for 12 weeks/3 months, unless otherwise instructed by Dr. Hage.
If your cervix was removed, do not use tampons or have sexual intercourse until after you have come for a post-op examination. If your cervix is still in place, you may resume sexual intercourse after 6 weeks unless instructed otherwise by Dr. Hage.
BOWELS:
It is normal not to have a bowel movement for several days after surgery. To avoid getting constipated, you may drink prune juice or take an over-the-counter product such as milk-of-magnesia or colace.
FOLLOW-UP APPOINTMENT:
If you do not have an appointment when you leave the hospital, call the office the next business day to arrange for an appointment within 2-3 weeks of your surgery.
IF YOU NOTICE ANY of the FOLLOWING:
• Fever > 100.4 on two occasions, 4 hours apart.
• Pus coming out of the incision.
• Vaginal bleeding heavier than a period.
• Pain that is not controlled by the prescribed medicines and/or does not lessen with time.
• Unable to keep down liquids.
• Redness, swelling or bruising around the incision which is worsening day-after-day.
YOU SHOULD:
• Call for a same day appointment
• Go to urgent care.
• Go to the Emergency Room.
To leave a non-urgent message for your physician, call the office.
This information is provided as a resource only and is not intended to be a recommendation or a substitute for consultation with Dr. Hage regarding your health and needs.
Hysterectomy – Robotic & Laparoscopic
WHAT TO EXPECT:
Your throat may be sore for a few days from the breathing tube that was used during surgery. You may also have abdominal and/or shoulder pain from gas that we used to inflate your belly during surgery. These symptoms are not serious. They will go away within a few days.
INCISIONS:
You have 3 or 5 small incisions in your belly. If the incisions are covered by gauze or a clear dressing, you can uncover them 24 hours after surgery. If you have tape strips over the incisions, leave them on for 7 days and then remove them. If you have glue, do not remove it until further instruction. When you shower, let soapy water run over the incisions. Afterward, pat them dry. If a strip starts to fall off, it’s okay to remove it. It is normal to have redness or bruising around the incisions.
PAIN:
You will get prescriptions for Ibuprofen (Motrin) and a narcotic pain pill (Norco or Tylenol #3.) Take Ibuprofen three times a day, with meals, until you no longer need it. If you need them, take the narcotic pain pills in addition, according to the instructions on the bottle.
DIET:
If you aren’t hungry, just drink liquids for the first 24 hours. When you are hungry, eat regular food. Drink plenty of water and eat lots of fruits and vegetables to avoid constipation. If eating regular foods gives you gas pains, go back to clear liquids.
ACTIVITY:
You can shower 24 hours after your surgery. Don’t drive for at least one week after surgery. After that, when you are no longer taking narcotic pain pills, not feeling drowsy, and you can move around quickly without discomfort, you may begin to drive. Don’t stay in bed all day. You will heal faster if you get up and move around the house. You may walk up and downstairs. It is not harmful. When you feel ready for a particular activity (such as light housework or exercise) you can try it. You can expect to be able to return to work approximately 1-6 weeks after your surgery.
VAGINAL DISCHARGE:
It is normal to have some bleeding or discharge from the vagina for a few weeks after surgery.
INTERCOURSE:
DO NOT PUT/INSERT ANYTHING INSIDE THE VAGINA. NO sexual intercourse for 12 weeks/3 months, unless otherwise instructed by Dr. Hage.
If your cervix was removed, do not use tampons or have sexual intercourse until after you have come for a post-op examination. If your cervix is still in place, you may resume sexual intercourse when your belly is not sore and when you feel ready, unless otherwise instructed by Dr. Hage.
BOWELS:
It is normal not to have a bowel movement for several days after surgery. If you feel constipated after that, you may drink prune juice or take an over-the-counter product such as milk-of-magnesia or Colace.
FOLLOW-UP APPOINTMENT:
If you do not have an appointment when you leave the hospital, call the office the next business day to arrange for an appointment within 2-3 weeks of your surgery.
IF YOU NOTICE ANY of the FOLLOWING:
• Fever > 100.4 on two occasions, 4 hours apart.
• Pus coming out of the incision.
• Vaginal bleeding heavier than a period.
• Pain that is not controlled by the prescribed medicines and/or does not lessen with time.
• Unable to keep down liquids.
• Redness, swelling or bruising around the incision which is worsening day-after-day.
YOU SHOULD:
• Call for a same day appointment
• Go to urgent care.
• Go to the Emergency Room.
To leave a non-urgent message for your physician, call the office.
This information is provided as a resource only and is not intended to be a recommendation or a substitute for consultation with Dr. Hage regarding your health and needs.
Hysterectomy – Vaginal
WHAT TO EXPECT:
Your throat may be sore for a few days from the breathing tube that was used during surgery. You may also have abdominal and/or shoulder pain from gas that enters your abdomen from having surgery. These symptoms are not serious. They will go away within a few days.
INCISIONS:
You will not have any visible incisions, your incision is inside the vagina. When you shower, avoid getting too much water inside the vagina. Do not sit in a bathtub, unless instructed to do so by Dr. Hage.
PAIN:
You will get prescriptions for Ibuprofen (Motrin) and a narcotic pain pill (Norco or Tylenol #3.) Take Ibuprofen three times a day, with meals, until you no longer need it. If you need them, take the narcotic pain pills in addition, according to the instructions on the bottle.
DIET:
If you are not hungry, just drink liquids for the first 24 hours. When you are hungry, eat regular food. Drink plenty of water and eat lots of fruits and vegetables to avoid constipation. If eating regular foods gives you gas pains, go back to clear liquids.
ACTIVITY:
You can shower 24 hours after your surgery. Don’t drive for at least 3 weeks after surgery. After that, when you are no longer taking narcotic pain pills, not feeling drowsy, and you can move around quickly without discomfort, you may begin to drive. Do not stay in bed all day. You will heal faster if you get up and move around the house. You may walk up and downstairs. It is not harmful. When you feel ready for a particular activity (such as light housework or exercise) you can try it. You can expect to be able to return to work approximately 3-4 weeks after your surgery.
VAGINAL DISCHARGE:
It is normal to have some bleeding or discharge from the vagina for a few weeks after surgery.
INTERCOURSE:
DO NOT PUT/INSERT ANYTHING INSIDE THE VAGINA. NO sexual intercourse for 12 weeks/3 months, unless otherwise instructed by Dr. Hage.
Do not use tampons or have sexual intercourse until after you have come for a post-op examination.
BOWELS:
It is normal not to have a bowel movement for several days after surgery. To avoid getting constipated, you may drink prune juice or take an over-the-counter product such as milk-of-magnesia or colace.
FOLLOW-UP APPOINTMENT:
If you do not have an appointment when you leave the hospital, call the office the next business day to arrange for an appointment within 2-3 weeks of your surgery.
IF YOU NOTICE ANY of the FOLLOWING:
• Fever > 100.4 on two occasions, 4 hours apart.
• Pus coming out of the incision.
• Vaginal bleeding heavier than a period.
• Pain that is not controlled by the prescribed medicines and/or does not lessen with time.
• Unable to keep down liquids.
• Redness, swelling or bruising around the incision which is worsening day-after-day.
YOU SHOULD:
• Call for a same day appointment
• Go to urgent care.
• Go to the Emergency Room.
To leave a non-urgent message for your physician, call the office.
Pelvic Repairs
WHAT TO EXPECT:
Your throat may be sore for a few days from the breathing tube that was used during surgery. You may also have abdominal and/or shoulder pain from gas that enters your abdomen from having surgery, if you also had a hysterectomy. These symptoms are not serious. They will go away within a few days.
INCISIONS:
You will not have any visible incisions, your incision is inside the vagina. You may have an incision similar to an episiotomy. When you shower, avoid getting too much water inside the vagina. Do not sit in a bathtub, unless instructed to do so by Dr. Hage.
PAIN:
You will get prescriptions for Ibuprofen (Motrin) and a narcotic pain pill (Norco or Tylenol #3.) Take Ibuprofen three times a day, with meals, until you no longer need it. If you need them, take the narcotic pain pills in addition, according to the instructions on the bottle.
DIET:
If you are not hungry, just drink liquids for the first 24 hours. When you are hungry, eat regular food. Drink plenty of water and eat lots of fruits and vegetables to avoid constipation. If eating regular foods gives you gas pains, go back to clear liquids.
ACTIVITY:
You can shower 24 hours after your surgery. Don’t drive for at least 3 weeks after surgery. After that, when you are no longer taking narcotic pain pills, not feeling drowsy, and you can move around quickly without discomfort, you may begin to drive. Do not stay in bed all day. You will heal faster if you get up and move around the house. You may walk up and downstairs. It is not harmful. When you feel ready for a particular activity (such as light housework or exercise) you can try it. You can expect to be able to return to work approximately 3-4 weeks after your surgery. With major prolapse repairs, avoid strenuous activity for 6-8 weeks to allow complete healing and avoid recurrence.
INTERCOURSE:
Do not use tampons or have sexual intercourse until after you have come for a post-op examination. You may resume sexual intercourse after 6 weeks unless instructed otherwise by Dr. Hage.
BOWELS:
It is normal not to have a bowel movement for several days after surgery. To avoid getting constipated, you may drink prune juice or take an over-the-counter product such as milk-of-magnesia or colace.
FOLLOW-UP APPOINTMENT:
If you do not have an appointment when you leave the hospital, call the office the next business day to arrange for an appointment within 2-3 weeks of your surgery.
IF YOU NOTICE ANY of the FOLLOWING:
• Fever > 100.4 on two occasions, 4 hours apart.
• Pus coming out of the incision.
• Vaginal bleeding heavier than a period.
• Pain that is not controlled by the prescribed medicines and/or does not lessen with time.
• Unable to keep down liquids.
• Redness, swelling or bruising around the incision which is worsening day-after-day.
YOU SHOULD:
• Call for a same day appointment
• Go to urgent care.
• Go to the Emergency Room.
To leave a non-urgent message for your physician, call the office.
This information is provided as a resource only and is not intended to be a recommendation or a substitute for consultation with Dr. Hage regarding your health and needs.
Tubal Ligation
WHAT TO EXPECT:
Your throat may be sore for a few days from the breathing tube that was used during surgery. You may also have abdominal and/or shoulder pain from gas that we used to inflate your belly during surgery. These symptoms are not serious. They will go away within a few days.
INCISIONS:
You have 1 or 2 small incisions in your belly. If the incisions are covered by gauze or a clear dressing, you can uncover them 24 hours after surgery. If you have tape strips over the incisions, leave them on for 7 days and then remove them. When you shower, let soapy water run over the incisions. Afterward, pat them dry. If a strip starts to fall off, it’s okay to remove it. It is normal to have redness or bruising around the incisions.
PAIN:
You will get prescriptions for Ibuprofen (Motrin) and a narcotic pain pill (Norco or Tylenol #3.) Take Ibuprofen three times a day, with meals, until you no longer need it. If you need them, take the narcotic pain pills in addition, according to the instructions on the bottle.
DIET:
If you are not hungry, just drink liquids for the first 24 hours. When you are hungry, eat regular food. Drink plenty of water and eat lots of fruits and vegetables to avoid constipation. If eating regular foods gives you gas pains, go back to clear liquids.
ACTIVITY:
You can shower 24 hours after your surgery. Do not drive for at least 24 hours after surgery. After that, when you are no longer taking narcotic pain pills, not feeling drowsy, and you can move around quickly without discomfort, you may begin to drive. Do not stay in bed all day. You will heal faster if you get up and move around the house. You may walk up and downstairs. It is not harmful. When you feel ready for a particular activity (such as light housework or exercise) you can try it. You can expect to be able to return to work approximately 1-3 days after your surgery.
INTERCOURSE:
Do not use tampons or have sexual intercourse until after you have come for a post-op examination. You may resume sexual intercourse after your next period and when you feel ready, unless otherwise instructed by Dr. Hage.
BOWELS:
It is normal not to have a bowel movement for several days after surgery. If you feel constipated after that, you may drink prune juice or take an over-the-counter product such as milk-of-magnesia or Colace.
FOLLOW-UP APPOINTMENT:
If you do not have an appointment when you leave the hospital, call the office the next business day to arrange for an appointment within 2-3 weeks of your surgery.
IF YOU NOTICE ANY of the FOLLOWING:
• Fever > 100.4 on two occasions, 4 hours apart.
• Pus coming out of the incision.
• Vaginal bleeding heavier than a period.
• Pain that is not controlled by the prescribed medicines and/or does not lessen with time.
• Unable to keep down liquids.
• Redness, swelling or bruising around the incision which is worsening day-after-day.
YOU SHOULD:
• Call for a same day appointment
• Go to urgent care.
• Go to the Emergency Room.
To leave a non-urgent message for your physician, call the office.
This information is provided as a resource only and is not intended to be a recommendation or a substitute for consultation with Dr. Hage regarding your health and needs.
Vaginal Delivery
WHAT TO EXPECT:
Your back may be sore for a few days from pushing or from the epidural, if you had one. You may also have muscle soreness from exertion during pushing. These symptoms are not serious. They will go away within a few days.
INCISIONS:
If you had an episiotomy or a laceration (tear) in the vagina, use the squirt bottle and rinse your stitches each time you use the bathroom. Use the Dermoplast spray and Tucks wipes as directed. It is often helpful to soak in a warm bathtub once a day.
PAIN:
You will get prescriptions for Ibuprofen (Motrin) and possibly a narcotic pain pill (Norco or Tylenol #3.) Take Ibuprofen three times a day, with meals, until you no longer need it. If you need them, take the narcotic pain pills in addition, according to the instructions on the bottle.
DIET:
If you are not hungry, just drink liquids for the first 24 hours. When you are hungry, eat regular food. Drink plenty of water and eat lots of fruits and vegetables to avoid constipation. If eating regular foods gives you gas pains, go back to clear liquids.
ACTIVITY:
Do not drive for at least 48 hours after delivery. After that, when you are no longer taking narcotic pain pills, not feeling drowsy, and you can move around quickly without discomfort, you may begin to drive. Do not stay in bed all day. You will heal faster if you get up and move around the house. You may walk up and downstairs. It is not harmful. When you feel ready for a particular activity (such as light housework or exercise) you can try it. You can expect to be able to return to work approximately 4-6 weeks after your delivery.
INTERCOURSE:
Do not use tampons or have sexual intercourse until after you have come for a post-partum examination. You may resume sexual intercourse after 6 weeks unless instructed otherwise by Dr. Hage. You may want to consider contraception prior to resuming sexual activity.
BOWELS:
It is normal not to have a bowel movement for several days after delivery. To avoid getting constipated, you may drink prune juice or take an over-the-counter product such as milk-of-magnesia or colace.
FOLLOW-UP APPOINTMENT:
If you do not have an appointment when you leave the hospital, call the office the next business day to arrange for an appointment within 2-3 weeks of your surgery.
IF YOU NOTICE ANY of the FOLLOWING:
• Fever > 100.4 on two occasions, 4 hours apart.
• Pus coming out of the incision.
• Vaginal bleeding heavier than a period.
• Pain that is not controlled by the prescribed medicines and/or does not lessen with time.
• Unable to keep down liquids.
• Redness, swelling or bruising around the incision which is worsening day-after-day.
YOU SHOULD:
• Call for a same day appointment
• Go to urgent care.
• Go to the Emergency Room.
To leave a non-urgent message for your physician, call the office.
This information is provided as a resource only and is not intended to be a recommendation or a substitute for consultation with Dr. Hage regarding your health and needs.
Newborn Circumcision
- * The gauze on the penis will soak off easily in the bath. Once it comes off, it does not need to be replaced.
- * If bleeding occurs, apply gentle pressure with your thumb and index finger, up to five (5) minutes. If excessive bleeding occurs, go to the emergency room.
- * Change diapers often so that urine and feces do not irritate the area.
- * Wash the penis gently with soap and water daily after the first 24 hours.
- * Apply Neosporin or generic triple antibiotic ointment around the circumcised area during the first week to help prevent irritation and infection of the surgical area and to help expedite healing.
* If you have further questions, please do not hesitate to call the office.
This information is provided as a resource only and is not intended to be a recommendation or a substitute for consultation with Dr. Hage regarding your health and needs.
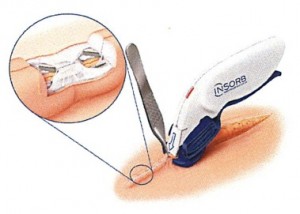
Absorbable Skin Staples
Dr. Hage cares about your ‘total surgical experience’, and uses absorbable skin staples to close your incision. These staples are place underneath the skin to create a comfortable and cosmetic incision closure. This rapid closure method reduces the time under anesthesia in surgery. Clinical studies show that the use of these absorbable staples may result in lower would complications than metal skin staples or suture, including Surgical Site Infections. Absorbable staples are not like metal skin staples that puncture the the skin resulting in increased pain and discomfort, and a less than optimal cosmetic results. And, metal staples must be removed post-operatively. Over 500,000 patients throughout the world have benefited from the INSORB Skin Closure Modality.
WHAT ARE ABSORBABLE SKIN STAPLES MADE OF?
Absorbable skin staples are made from the same types of polymers as many of the absorbable sutures. In this case, absorbable staples are comprised of a co-polymer of polylactic acid and poly glycolic acid. This co-polymer has a well-established clinical history as a safe and effective closure material.
Tissue studies have shown that the absorbable staple polymer is very benign and causes a lower inflammatory response compared to certain absorbable suture materials.

HOW DO ABSORBABLE STAPLES DEGRADE & HOW LONG DOES IT TAKE?
Just like absorbable sutures, absorbable staples degrade by a process of heat and hydrolysis. What happens is the body gets the staples ‘wet’ and the body’s elevated temperature begins the process of ‘breaking down’ the materials. Typically, the absorbable staples are essentially absorbed (i.e., less than 40% of the original weight) within 90 to 120 days. Eventually, the dissolved polymer is safely absorbed and excreted by the body.
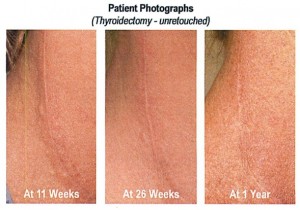
IS IT NORMAL TO FEEL OR SEE TINY BUMPS ON MY INCISION?
Depending on the skin thickness and the location of the incision, it may be possible to see or feel tiny ‘bumps’ under the skin which may be apparent for a number if months. DO NOT be concerned: “the ‘bumps’ will disappear after the staples are fully absorbed. Below are photos of a surgical incision closed with absorbable staples in the very thin neck tissue. These photos clearly demonstrate that even in this extreme situation, staples were absorbed by six months, and the feel and appearance of the incision continuously improved.